ABC Heart Fail Cardiomyop 2022; 2(2): 138-145
Association of Age with Optimal Medical Therapy in Patients with Chronic Heart Failure
Abstract
Background:
The adherence to guideline-directed medical therapy in patients with heart failure (HF) remains suboptimal.
Objectives:
We evaluated the association between age and adherence to guideline-directed medical therapy in patients with chronic HF and explored whether polypharmacy and comorbidities might explain this association.
Methods:
We performed a cross-sectional study of 374 patients with chronic HF and left ventricle ejection fraction < 50% (23 to 89 years old, 33% women) between 2018 and 2019. GDMT was defined as using HF-related disease-modifying medications at the target dose according to guidelines. Patients were classified in 3 age groups (23 to 57, 58 to 67, and 68 to 89 years old).
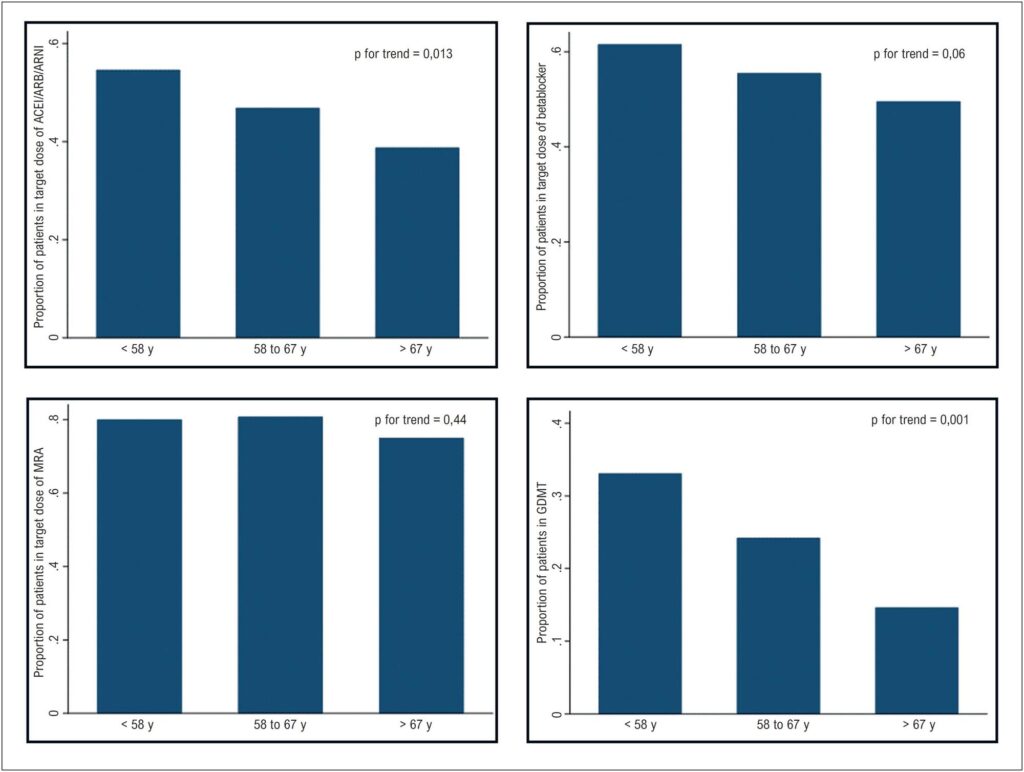
Results:
Older patients were less likely to receive optimal therapy (33% versus 24% versus 15%, p < 0.001 for each age category, respectively). After adjusting for potential confounders, the chances of receiving medical therapy at optimal dose significantly reduced for each age-decade increase (OR 0.66 [95% confidence interval 0.48 – 0.92], p = 0.013). The proportion of this association that was explained by polypharmacy (0% [0% – 3.5%]) or comorbidities (7% [0% – 41%]) was negligible.
Conclusion:
We found that age was inversely associated with optimal drug therapy for HF, and polypharmacy or comorbidities do not appear to explain this.
Keywords: Aging; Drug Therapy; Heart Failure; Polypharmacy
688